The acoustic neuroma (or schwannoma) is a benign tumor which originates from the sheath covering the eighth cranial nerve (vestibular-cochlear). This nerve, exclusively sensory, consists of two separate nerves: the cochlear (acoustic) nerve responsible for the perception of hearing and the vestibular nerve responsible for the balance. In turn, the vestibular nerve is constituted by a superior per branch, which runs in close contact with the facial nerve, and an inferior branch, which runs just above the cochlear nerve. This nerve arises from the cochlea, while the superior and inferior vestibular nerves arise from the organs responsible for the balance (vestibule, semicircular canals, saccule and utricle).
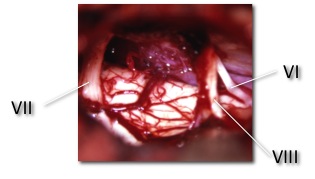
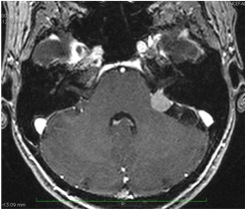
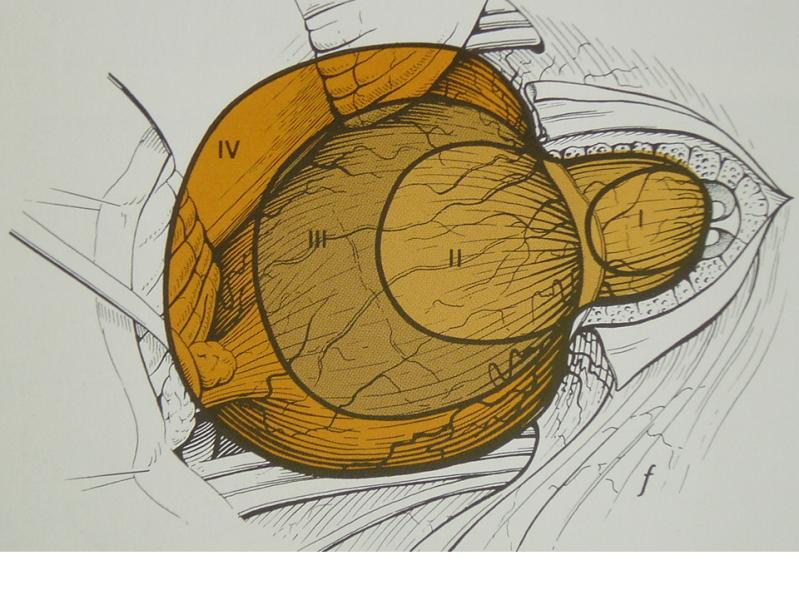
The 4 nerves in question (2 vestibular, cochlear and facial) run through a small bony canal (internal auditory canal) for about 1 cm before entering in the cerebellopontine angle and reaching the entry zone in the brain stem, part of the brain where originate the majority of cranial nerves. The seventh cranial nerve, that is the facial nerve, is responsible for the movement of the ipsilateral hemiface and runs along the internal auditory canal together with the cochlear and vestibular nerves and the blood vessels.
The neuroma of the 8th cranial nerve (improperly said acoustic neuroma) originates from the covering sheath (myelin sheath of Schwann) of one of the two vestibular nerves (in over 70% of cases from the inferior), generally inside the internal auditory canal.
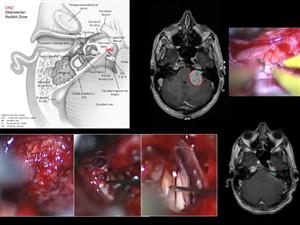
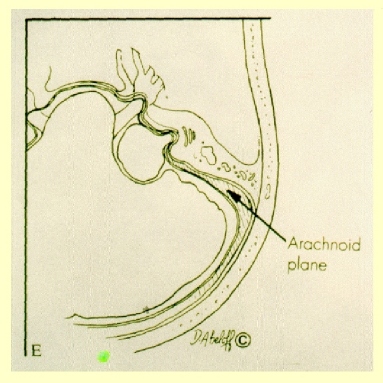
As regards the surgical treatment of this neoplasm, we routinely use the microsurgical technique (microsurgery), that is the surgical technique that is used working with the surgical microscope. It consists of careful and precise movements and gestures, which are made using dedicated instruments. The thorough knowledge of anatomy and the microsurgical continuous exercise (on the patient and, above all, on anatomical specimens) allow the skull base microneurosurgeon to get the best results in terms of removal of the tumor and morbidity.
In Neurosurgical Departments with medium-high experience, the acoustic neuromas surgical mortality is close to zero, and in those rare cases when it happens, there are usually huge neuromas, very adherent to the brain stem and/or with hydrocephalus.
For what concerns morbidity associated with this surgical procedure, it seems correct to talk about it in a different way, in relation to the size of the neuroma, its extension and relations with the brain stem.
1. The small intracanalar neuromas (less than 1 centimeter) with hearing preserved totally or in substantial part, represent the better situation for the complete removal of tumor and the preservation of the facial and acoustic nerves. However, it seems reasonable also the “wait and see” choice approach, with clinical and MRI monitoring every 6-12 months.
If the hearing is lost completely the choice of waiting is even more suitable, leaving the surgical solution for those cases in which the tumor starts to grow on the scheduled MRI controls.
For what concerns the surgical approach used for the removal, in patients with preserved hearing, the retrosigmoidal approach is preferred, while in patients with complete hearing loss the best way is usually the transmastoid-translabyrinthine approach, that does not expose the brain. Although this second path is usually a competence of ENT surgeons, several Neurosurgeons (including me) have acquired during the years the necessary experience to remove the tumor with both approaches.
2. The intra-extracanalar neuromas (protruding in the cerebellopontine angle) below the 2 cm in diameter, with partially or completely absent hearing, should be treated by the retrosigmoid approach. The possibility to save the the facial nerve are higher than 90%, although a slight transient paresis of the nerve can be observed in one patient out of three, with recovery within 3-6 months (experience not only personal but also of great neurosurgeons like Fukushima, Samii, and others). In patients with quite normal hearing, the possibility of conservation of this function is hovering around 50% and decreases in inverse proportion to the size of the neoplasm. If then there is tinnitus it is almost impossible to save the cochlear nerve that, on the contrary, is better to cut in order to avoid the persistence of tinnitus after surgery even in the absence of hearing.
The difficulty encountered in saving the cochlear nerve is linked to the fact that, as mentioned earlier, the neuroma arises in over 70% of cases from the inferior vestibular nerve, in close contact with acoustic nerve that for this reason is the first to be involved. In 20-25% of cases the neuroma arises from the superior vestibular nerve, in close contact with the facial nerve. These are the cases where it is really difficult to avoid a temporary or permanent deficit of the facial nerve, fully wrapped by the tumor.
If the total removal has a high probability of causing a permanent deficit of the facial nerve, in agreement with the patient, it is usually advisable to leave a small piece of tumor capsule on the nerve and to follow their evolution by periodic MRI. Takanori Fukushima, international expert in this field, reports to adopt this strategy in around 30% of patients. In cases with hearing function completely lost is preferred to use the extracranial translabyrinthine approach. Even in these cases the percentage of deficit of the facial nerve are in line with what was said earlier.
3. In patients suffering from neuromas with a 2 – 2.5 cm diameter preserving the acoustic nerve is usually very difficult. Although the cochlear nerve may in many cases remain intact at the end of surgery, it generally does not work. The possibility to preserve the facial nerve falls to 70-80%, while a slight transient paresis is observed in almost half of the patients. In these cases too it may be decided in the presence of a tight tumor adhesion to the facial nerve to leave a small fragment of capsule of neuroma on the nerve and to follow-up it periodically. This is because it is possible that a tiny residue over time could slowly grow back. In any case, the possibility of recurrence of the disease is possible, but rare, because of with the surgical excision is removed most of the vascular supply to the tumor. In case of recurrence of the lesion (which develops during the course of many years) it is possible to reconsider a second surgical treatment.
4. In giant neuromas (over than 3 cm of maximum diameter) relations with the brainstem make the surgical removal (usually by retrosigmoid approach) very delicate and beyond the risk of damage for the cranial nerves (in these cases, in addition to facial and cochlear nerves may sometimes occur trigeminal deficiency and difficulties in swallowing already during the preoperative) there is a chance of problems, even at the expense of brainstem. In these patients the removal must be judicious and then consider the possibility of a “safe” subtotal removal. In these conditions may also be associated an obstructive hydrocephalus, which often improves after surgery, but sometimes needs to be derived with a ventriculo-peritoneal shunt.
Written by Luciano Mastronardi
Advice from normal hearing suffering from acoustic neuroma
References :
https://www.youtube.com/watch?v=nYhuc2imIfY&feature=youtu.be
Attachments :
Positon of facial nerves in acoustic neuromas
Microanatomy and Dissection of The Temporal Bone
CE-Chirp® ABR in cerebellopontine angle surgery neuromonitoring