Low back pain
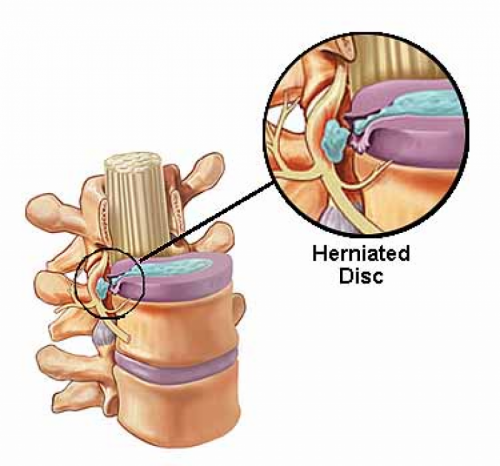
Herniated disc
Article written by : Raffaele Roperto
What is meant by the terms low back pain and sciatica?
Acute low back pain (LBP) with or without radiation to the lower limbs (sciatica or cruralgia) is a frequent symptom among the population and in most cases it resolves spontaneously.
However, it may be associated with lumbar intervertebral disc herniation in addition to systemic diseases, inflammatory, neoplastic, or infectious involving the spine. (Fig. 1)
Is it a frequent disease?
The symptomatic lumbar disc herniation can cause back pain, a condition that in Western Countries affects 90% of the adult population during the course of their lives, and that is a frequent cause of functional limitation, more or less incapacitating below 45 years of age.
In 1999, ISTAT survey revealed that 8,2% of the Italian population reported to be suffering from sciatica, approximately 7.3% of males and 9.3% females. (Fig. 2)
Are there risk factors and / or more susceptible categories?
The disc herniation associated with clinical symptoms occurs most often in people aged 30-50 year-old. Risk factors: sedentary occupations and physical inactivity, overweight, tall stature, long and steady motor vehicles driving, vibration, jobs with high physical effort especially if they involve manual handling of loads , and pregnancies. (Fig. 3)
How can you orient yourself to understand what you have is more than just a backache?
The indicators are:
• persisting back pain and / or lombosciatlagia or cruralgia
• unilateral or bilateral hyposthenia
• hypoesthesia or anesthesia along the lower limbs or saddle in the perianal region
• retention or urinary incontinence and / or fecal
How to get to a diagnosis?
By specialist examination, during which the patient is subjected to several clinical trials, including: SLR (Straight Leg Raising); Lasègue maneuver, Wasserman maneuver, sitting knee extension test, sock test; slump test, weakness of the extension plantar of the ankle; front flexion of the chest. Thus: execution of an lumbosacral MRI, T1 and T2 weighted sequences on both sagittal and axial views, sagittal view of the intervertebral foramina bilaterally, images equal to or less than 1 mm of thickness; a diagnostic completion with standard radiographs and / or dynamic of the lumbosacral spine will be necessary when MRI documents the presence of spinal instability.
Treatment, which and when!
The surgery of the disc herniation can be very rewarding for both the surgeon and the patient, who enters the operating room in the throes of excruciating pain and can get out of it completely relieved. The national plan guideline of the Ministry of Health 2005 suggests the surgical indication in case of “syndrome of the cauda aequina” progressive motor deficit and lombosciatlagia iperalgica with intractable pain and also resistant to opiates.The treatments used for symptomatic lumbar disc herniation can be classified into:
• surgical procedures (standard discectomy, microdiscectomy, automated percutaneous dicectomy, discectomy with laser or coblation, replacement of the intervertebral disc)
• minimally invasive interventions (chemonucleolysis, epidural steroid injections, intradiscal electrothermal therapy, or IDET, intradiscal oxygen and ozone)
• conservative treatments (non-epidural medications, physiotherapy, massage, traction, spinal manipulation, postural education school or back school).
Moreover, the national plan guideline 2005 shows that the “standard discectomy or microdiscectomy represent selected surgical techniques; interventions of chemonucleolysis are not advisable, considering the reduced efficacy compared to discectomy; the use of acetaminophen or NSAIDs is recommended to alleviate painful symptoms , but only for not prolonged periods of time”.
The spine surgery, however, is not without risks and perioperative complications and the consequent permanent damage can be awaited, including failed-back syndrome. The ISTAT data indicate that the rate of reinterventions from one to ten years ranges from 2.5% to 6%.
References :
Attachments :




