Intracerebral tumors
Resection of brain tumors in eloquent areas
In the San Filippo Neri Hospital in Rome, since some several years, in selected cases we perform brain surgery with the patient awake during the crucial phase of the procedure of removal, especially for tumors affecting the area of the language, in order to perform the stimulation of this centers and to confirm their anatomical location, with cooperation of the awake patient.
Our experience is in line with that of the international centers of reference (article attached). Below there is the abstract of a paper we presented at a conference. Hopefully it will be of interest and help.
Surgery “asleep-awake-asleep” (awake surgery) for the treatment of intracerebral tumors in eloquent areas. Importance of cortical and subcortical mapping.
Luciano Mastronardi (Director of Neurosurgery)
, Alessandro Cerroni (Intensive Care/Neurosurgical Anesthesiology)
.
San Filippo Neri Hospital, Rome.
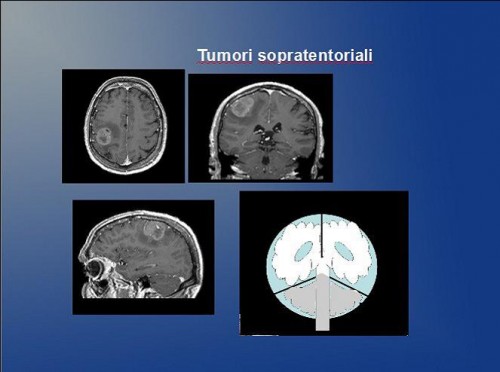
Primitive intracranial tumors are relatively uncommon, about 10 cases per 100,000 inhabitants per year. Most of them originate from nutritional and support tissues (glia) in which are located neurons and nervous fibers (gliomas), from the meninges (meningiomas), and from the myelin sheath of cranial nerves (neuromas). The brain tumor does not metastasize, except in rare cases. The ” benignity” of some organic intracranial tumors does not always correspond to the possibility of healing. In fact, in some locations, even the partial removal of the tumor can be very risky for the non-negligible mortality (as far as lesions adjacent to or contained into the brain stem), or the possible morbidity, as in the case of tumors arising in proximity of “eloquent” brain areas, (that express a particular function, such as language or motion), of the cranial nerves (optic, oculomotor, trigeminal, facial, acoustic, vagus, etc.), or encasing large arteries and veins of vital relevance.
Gliomas represent more than 50% of all intracerebral tumors and 2/3 of them are malignant. Gliomas, even if of a low-grade malignancy, tend to infiltrate the surrounding brain tissue, making typically radical removal very difficult. In fact, often functionally relevant cortical and subcortical areas may be localized within the tumor and function normally, the fact that implies the risk of a permanent deficit after resection of the tumor.
Intracranial awake surgery (asleep – awake – asleep)
The purpose of the modern neurosurgeon is to remove as much tumor as possible without causing additional and permanent neurological damage, minimizing the approach with the help of the neuronavigational system and of the operating microscope and using stimulation techniques and intraoperative cortical and subcortical mapping.
The mapping is very reliable if performed after extubation and awakening of the patient during the operation (after the removal of bone flap and opening the dura) and is particularly useful for identifying and preserving cortical areas of language and movement and subcortical fiber tracts, taking advantage from the patient cooperation.
Once the mapping of speech area has been completed, the patient is re-intubated by the endotracheal route with a fast track and a fiber optic laryngoscope and the “safe” removal of the tumor continues under general anesthesia until the end of surgery, with greater comfort for the patient.
Awake surgery is performed in a few centers in Italy, including Neurosurgery of the San Filippo Neri Hospital in Rome. In appropriately selected cases, this technique has allowed us to “maximize” the extent of removal of astrocytomas and brain gliomas in functionally eloquent areas, improving the quality of life and extending the survival. Although the preoperative mapping with functional MRI and PET is very useful, they are not considered enough reliable, especially for the areas of language. Therefore, the intraoperative cortical stimulation in the awake patient allows to precisely identify the sites of language and the motor areas, and thus to safe them. Performing the intervention by using the technique asleep-awake-asleep the discomfort for the patient is minimized.
References :
http://www.youtube.com/watch?v=jC4DABllVK8&feature=youtu.be
Attachments :
Awake surgery




